Introduction
Pulmonary tuberculosis (TB) and pneumonia are both respiratory diseases that primarily affect the lungs. Despite their similarities in symptoms, they have different causative agents, pathophysiology, diagnostic approaches, treatment protocols, and epidemiology. Understanding these differences is essential for proper diagnosis, treatment, and management of the conditions.
Causes and Pathogens
Pulmonary tuberculosis is caused by the bacterium Mycobacterium tuberculosis. It is an infectious disease that spreads through airborne droplets when an infected person coughs, sneezes, or speaks. The bacteria can remain dormant in the body for years before causing active disease, particularly in individuals with weakened immune systems.
Pneumonia, on the other hand, is an acute infection of the lung parenchyma that can be caused by a variety of pathogens, including bacteria, viruses, fungi, and even parasites. Common bacterial causes include Streptococcus pneumoniae, Haemophilus influenzae, and Klebsiella pneumoniae. Viral pneumonia can be caused by influenza viruses, respiratory syncytial virus (RSV), and, more recently, SARS-CoV-2, which is responsible for COVID-19. Fungal pneumonia is more common in immunocompromised individuals, such as those with HIV/AIDS or those undergoing chemotherapy.
Mode of Transmission
Pulmonary tuberculosis spreads primarily through airborne transmission. When an infected person expels bacteria into the air, others who inhale these droplets may contract TB. However, not everyone exposed to TB bacteria will develop active disease; some may remain asymptomatic carriers (latent TB infection).
Pneumonia transmission depends on its cause. Bacterial pneumonia can spread through respiratory droplets, contaminated surfaces, or aspiration of bacteria from the mouth and throat into the lungs. Viral pneumonia spreads through close contact, inhalation of respiratory droplets, or direct contact with contaminated hands or surfaces. Fungal pneumonia typically arises from inhaling spores from the environment.
Symptoms and Clinical Presentation
Both pulmonary tuberculosis and pneumonia present with respiratory symptoms, but they exhibit distinct characteristics:
Pulmonary Tuberculosis Symptoms:
- Chronic cough (lasting more than three weeks, often with bloody sputum)
- Night sweats
- Weight loss and loss of appetite
- Low-grade fever
- Fatigue and malaise
- Chest pain (occasionally)
- Shortness of breath (in advanced cases)
Pulmonary TB symptoms tend to develop gradually over weeks or months, leading to chronic deterioration in health if untreated.
Pneumonia Symptoms:
- Sudden onset of high fever and chills
- Productive cough (often with yellow, green, or rusty sputum)
- Shortness of breath and difficulty breathing
- Chest pain (pleuritic pain) that worsens with deep breathing or coughing
- Fatigue and muscle aches
- Confusion (particularly in elderly patients)
Unlike TB, pneumonia presents acutely, with rapid progression of symptoms over days.
Diagnosis
The diagnostic approaches for TB and pneumonia differ significantly.
Diagnosis of Pulmonary Tuberculosis:
- Tuberculin Skin Test (TST) / Mantoux Test – A delayed hypersensitivity test to detect TB exposure.
- Interferon-Gamma Release Assays (IGRAs) – Blood tests to detect latent TB infection.
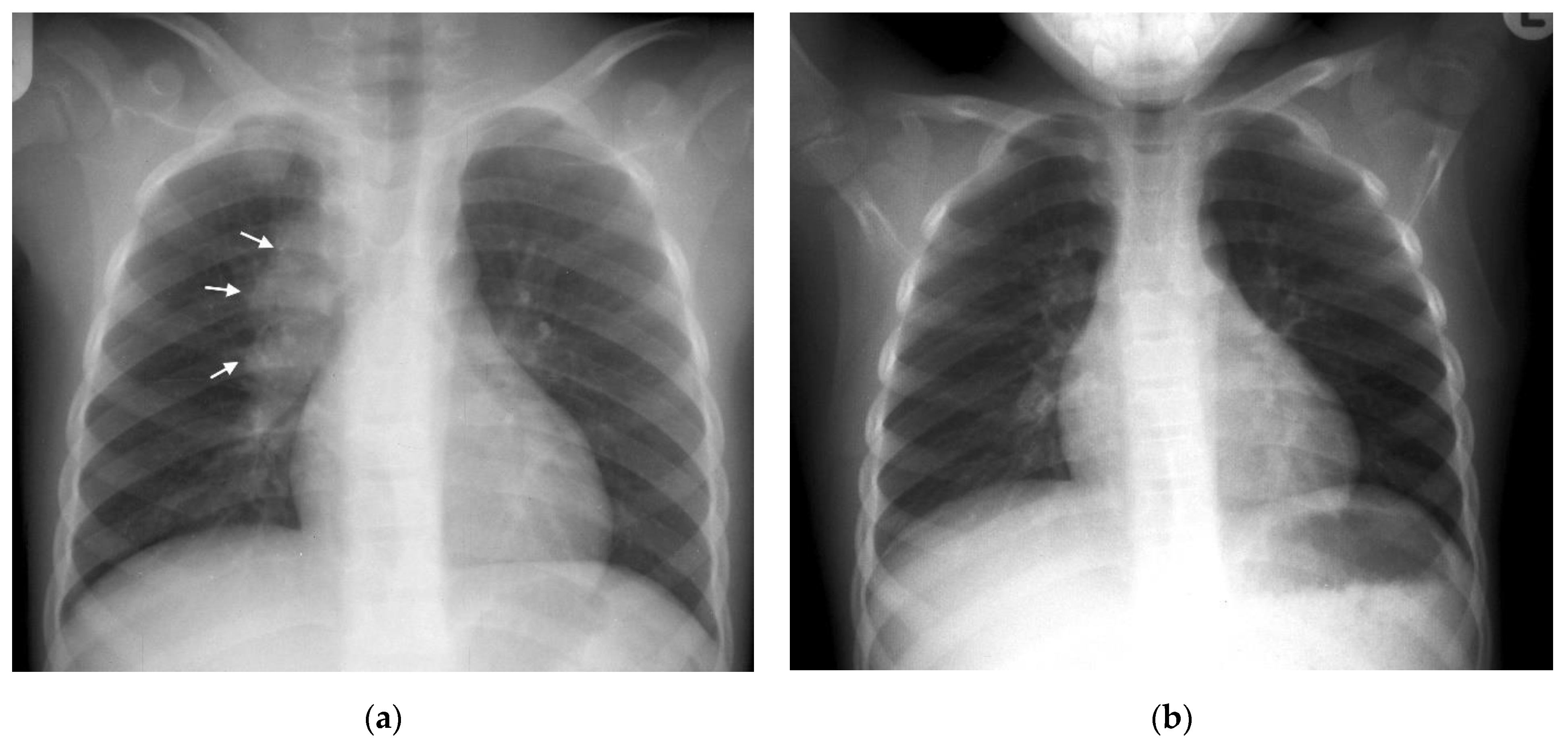
- Chest X-ray – Shows characteristic findings like upper lobe cavitary lesions or infiltrates.
- Sputum Microscopy & Culture – Acid-fast bacilli (AFB) staining and culture confirm active TB.
- GeneXpert MTB/RIF Test – A rapid molecular test that detects Mycobacterium tuberculosis and resistance to rifampicin.
Diagnosis of Pneumonia:
- Chest X-ray – Shows lobar or patchy infiltrates, which are suggestive of pneumonia.
- Complete Blood Count (CBC) – Indicates infection with elevated white blood cells.
- Sputum Culture and Gram Stain – Identifies the causative bacterial agent.
- Blood Cultures – Detects bacteremia in severe cases.
- Pulse Oximetry / Arterial Blood Gas (ABG) – Assesses oxygenation levels in severe pneumonia cases.
- PCR and Rapid Antigen Tests – Used for viral pneumonia diagnosis, especially in influenza or COVID-19 cases.
Treatment Approaches
The treatment strategies for TB and pneumonia vary significantly due to differences in their causative agents.
Pulmonary Tuberculosis Treatment:
TB treatment requires long-term antibiotic therapy due to the slow-growing nature of Mycobacterium tuberculosis.
- First-line TB drugs:
- Isoniazid (INH)
- Rifampicin (RIF)
- Ethambutol (EMB)
- Pyrazinamide (PZA)
- Treatment Duration: 6 months (intensive phase of 2 months followed by a continuation phase of 4 months)
- Drug-resistant TB: Requires second-line drugs such as fluoroquinolones or bedaquiline and extends treatment duration to 9-24 months.
Pneumonia Treatment:
Treatment varies based on the pathogen involved:
- Bacterial pneumonia: Treated with antibiotics like amoxicillin, azithromycin, or fluoroquinolones.
- Viral pneumonia: Supportive care with antivirals (e.g., oseltamivir for influenza, remdesivir for COVID-19).
- Fungal pneumonia: Treated with antifungals like amphotericin B or fluconazole.
- Hospitalized pneumonia cases: May require supplemental oxygen, IV fluids, and mechanical ventilation in severe cases.
Complications
Complications of Pulmonary Tuberculosis:
- Lung fibrosis and permanent lung damage
- Tuberculous meningitis
- Miliary TB (disseminated TB affecting multiple organs)
- Pleural effusion or pneumothorax
- Multi-drug resistant TB (MDR-TB) and extensively drug-resistant TB (XDR-TB)
Complications of Pneumonia:
- Acute respiratory distress syndrome (ARDS)
- Sepsis and organ failure
- Lung abscess or empyema (pus accumulation in the pleural cavity)
- Respiratory failure requiring ventilatory support
Prevention Strategies
Preventing Pulmonary Tuberculosis:
- BCG Vaccine (Bacillus Calmette-Guérin) for newborns in endemic areas
- Early detection and treatment of TB cases
- Infection control measures (masks, ventilation, isolation of infectious patients)
- Latent TB treatment for high-risk individuals
Preventing Pneumonia:
- Vaccination: Pneumococcal vaccine (PCV13, PPSV23), influenza vaccine, COVID-19 vaccine
- Hand hygiene and respiratory hygiene
- Smoking cessation to improve lung health
- Proper nutrition and hydration to strengthen immunity
Conclusion
While both pulmonary tuberculosis and pneumonia are serious respiratory diseases, they differ significantly in their causes, symptoms, diagnostic methods, treatment strategies, and prevention measures. TB is a chronic bacterial infection that requires long-term antibiotic therapy, whereas pneumonia is an acute infection that can be bacterial, viral, or fungal, often treated with shorter courses of antibiotics or antivirals. Early diagnosis and appropriate treatment are crucial for managing both diseases and preventing complications. Public health measures, including vaccination, proper hygiene, and infection control, play vital roles in reducing the global burden of these respiratory illnesses.


0 Comments